PCL injury – patient guide
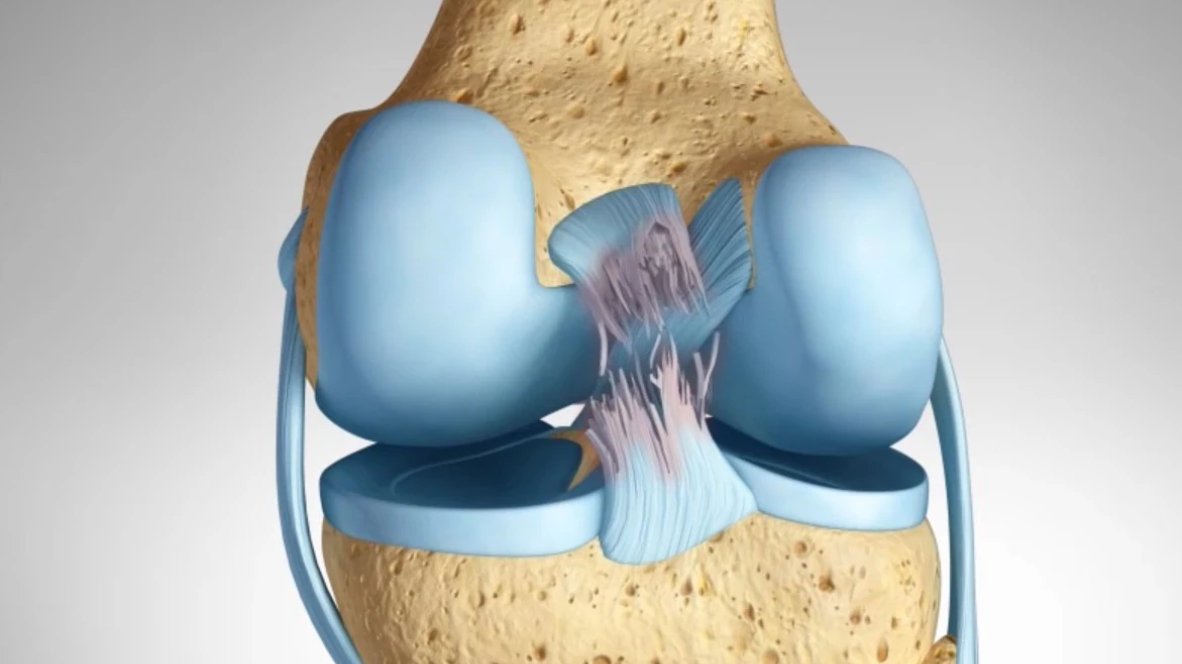
The Posterior cruciate ligament (PCL) is located in the back of the knee . It is one of the ligaments connecting femur (thigh bone) to tibia (shin bone ) and is the primary restraint to posterior translation of the tibia.
Injury to this ligament requires a powerful force ; such as a dashboard injury during a car accident or during contact sports .
This injury may occur in isolation (40%) or along with tears to other
The thigh bone (femur ) and shin bone (tibia) together form the knee joint with the knee cap (patella) sitting in front. The joint is connected and stabilised with the help of four main ligaments .
The collateral ligaments control any unusual sideways movement. The medial collateral ligament (MCL) on the inside and Lateral collateral ligament (LCL) on the outside.
The cruciate ligaments cross each other like an X . Anterior cruciate ligament in the front and posterior cruciate ligament in the back ;preventing back and forth movements.
PCL is the primary restraint to posterior shinbone(tibia) translation at 90 degrees of flexion and to certain extent prevents excessive outward twisting.
The anterolateral(larger) band of PCL is tight when knee is bent and posteromedial (smaller) is tight while the knee is straighter.
Injury to the PCL will cause buckling and may also result in damage to the joint leading to arthritis .
Clinical history
Commonly seen after dashboard injury in car accidents , contact sports; this injury may be neglected as being trivial initially . Patients may notice swelling around the knee , it may feel wobbly especially during sudden direction change or even more easily in combined injuries .
Pain may worsen over time while walking and climbing down stairs, more in the front or insides of the knee joint.
Clinical exam
The physician will examine the patients gait, alignment of the limb , swelling , bruises , movement and check for instability with special tests such as Posterior drawer test , Lachhman test , quadriceps active test, reverse pivot shift test .
The posterolateral complex is evaluated using dial test, posterolateral drawer test , ER recurvatum test .
Missing a combined PCL-PLC injury in the knee may lead to deleterious results of the PCL Reconstructed knee.
Routinely standard X-rays of the knee (AP/Lateral and skyline ) are asked for,
Stress X-rays( where the shin bone is pushed and pulled ) to determine the extent of laxity , help in grading and decision making.
In chronic injuries ,long leg X-rays(scannograms) ascertain alignment.
MRI (magnetic resonance imaging ) helps on diagnosis of these tears along with injuries to other ligaments , menisci or cartilage.
The injury is then graded according to clinical and radiological findings.
Grade 1 Sprains. The ligament is mildly damaged in a Grade 1 Sprain. It has been slightly stretched, but is still able to help keep the knee joint stable.
Grade 2 Sprains. A Grade 2 Sprain stretches the ligament to the point where it becomes loose. This is often referred to as a partial tear of the ligament.
Grade 3 Sprains. This type of sprain is most commonly referred to as a complete tear of the ligament. The ligament has been split into two pieces, and the knee joint is unstable.
Treatment rationale
Partial isolated tears are treated non operatively .
Complete PCL tears treated non operatively increase the risk of degenerative changes of the knee joint .
Surgical is recommended for complete and combined PCL injuries to restore joint stability and improve function .
Non operative treatment
The inherent healing capacity of PCL allows for non operative treatment . The drawback is that it may heal in a lax position .
Dynamic PCL braces allow for proper healing of the ligament
If non operative treatment fails operative treatment is indicated
Operative treatment
This is mostly done using arthroscopic technique wherein a new graft graft is created using patients own tendon or a donor graft .
Firstly the graft is harvested and prepared from the donor site . Commonly used graft are the semitendinosus and gracialis tendons or the bone patella tendon bone graft .
Tunnels are drilled in tibia(shinbone) and femur ( thigh bone) and the graft is passed. Eventually secured with buttons and screws .
Different techniques such as single bundle , double bundle , inlay techniques have been used and described for PCL reconstruction .
Post op rehabilitation
Post operatively the patient is placed in a brace with special accommodation to prevent the sagging of shinbone and subsequent laxity .
PCL brace is worn Upto 6 months post operatively.
Patient is allowed progressive weight bearing with walker. Upto 6 weeks of non weight bearing is recommended .
Early quadriceps strengthening exercises are done . Progressive goal oriented rehabilitation program is given in 5 phases .
Phase I – 0 to 6 weeks after surgery, is marked by progressive range of motion (ROM) exercises beginning with passive prone ROM from 0 to 90 degrees of knee flexion for the first 2 weeks after surgery advancing to full passive prone ROM as tolerated. During this phase, it is critical to prevent hyperextension and posterior tibial translation to protect the healing PCL graft from elongating.
Phase II, from 7 to 12 weeks postoperatively, involves similar precautions with progression to crutch weaning and weightbearing activities as tolerated, while restricting the knee to less than 70o of flexion during weightbearing exercises.
Brace use continues in phase III, from 13 to 18 weeks after surgery, with ROM weight-bearing exercise progressing past 70o of knee flexion after 16 weeks.
Phase IV, 19 to 24 weeks postoperatively, is characterized by the gradual introduction of sport-specific drills.
In phase V, 25 to 36 weeks after surgery, the patient may begin to wean from brace use if the 6 month postoperative
PCL stress radiographs demonstrate sufficient healing and begin a straight-line jogging progression with the eveNtual return to preoperative activities.
